COVID-19
While COVID-19 isn’t just affecting GBTQ2S guys, there are ways that the Canadian and Ontario pandemic response affects us in particular. We put together this page to cover some of those ways and connect you to resources that might be helpful.
- Sex in a pandemic
- Handling isolation
- Drug use / PnP in a pandemic
- How are GBTQ2S men affected?
- Showing up for each other
- What is COVID-19?
- Resources
As a community, cis and trans gay, bi, queer, and two-spirit men are no strangers to being excluded or treated differently by governments and public health authorities. While much of this discrimination was (and is) based on stereotypes, homophobia/transphobia, and colonialism, it also comes from them not understanding or valuing how our communities are different. When these messages don’t speak directly to our lives and the challenges we face, it becomes easier for some of us to tune them out.
GBTQ2S guys have a long history of navigating a complex world of sexual choices. That has been true throughout the HIV/AIDS epidemic and it’s true now through this pandemic. Our communities and individual choices are complex and our lives are often complicated. There is no single right choice that applies to all of us equally, but there are things that we should all know when it comes to weighing the choices we make and the options available to us. The biggest one being that this pandemic is real, it can be deadly, and it takes all of us doing our best to help protect as many people as possible including our own health.
Ultimately, we’re all responsible for our own actions and for the consequences of those actions. We hope this information helps you to navigate these choices and to keep you safe and connected throughout this unpredictable and rapidly changing situation.
We’ll keep it updated when new information is available. If you come across a resource or information that you think might be helpful, please let us know.
Sex in a pandemic
COVID-19 is not a sexually-transmitted infection, but it is highly contagious. It can be passed on through droplets (spit, mucous) if you’re in close contact with someone—even if you don’t have symptoms. So, if you’re close enough to fuck, you’re close enough to get or pass on COVID-19.

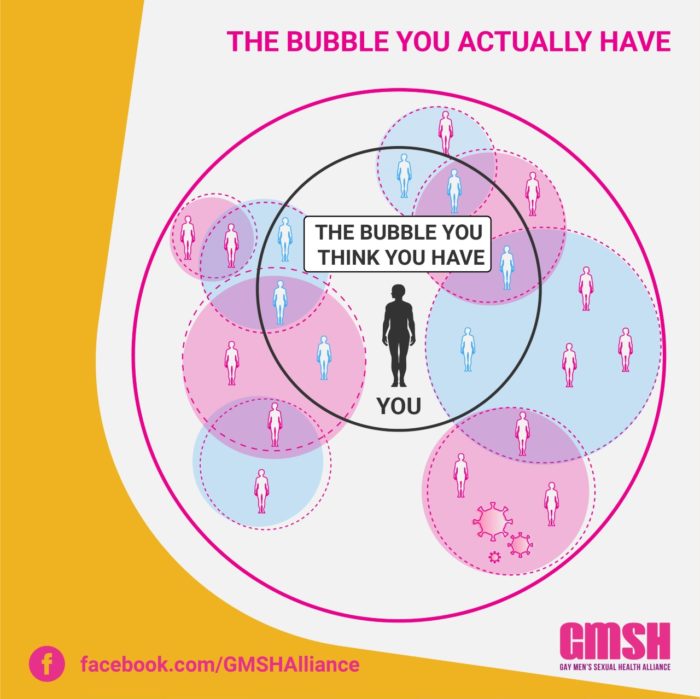
The “shared bubble”
With COVID-19 cases rising in Ontario, and the possibility of some places moving back into Phase 2 with restricted movement, you’ll want to think carefully about who really is in your shared bubble. The people that you see regularly—that you share indoor space with (or intimate space with)—are the ones most likely to pass on or contract COVID. Keeping a shared bubble is about limiting the possible spread of the virus and closing the loop of close interactions.
It’s possible to make an arrangement with another person to join each others’ bubble in order to not be alone. So if you live alone and are isolating and you pair up with someone else who is also isolating, then you effectively become one contained unit. If you’re travelling between spaces, take all of the usual precautions including washing your hands thoroughly. This kind of arrangement only works if there is openness, honesty, communication, and trust.
If you have a partner that you don’t live with (or a regular fuck buddy), this “shared bubble” approach might be a way for you to manage isolation in the coming weeks and months. Just know that the more people who are involved (including a partner’s roommates, family, or co-workers), the greater the risk of spreading or contracting COVID-19. So what might seem like a closed bubble of five people across three differen t households can easily grow to be 65 or 70 people once everyone else’s connections are counted.
What about glory holes?
As with any close contact, using a glory hole isn’t completely risk-free in terms of COVID transmission. But using a barrier can be one way to reduce potential exposure. More than just being a gag, the great folks at the BC Centre for Disease Control have recommended that using a barrier that allows for sexual contact, but limits face-to-face contact, are worth considering. It’s worth noting that Public Health Ontario hasn’t included this messaging in their guidelines.
If you are going to use a glory hole, remember to follow other guidelines as well—don’t exchange saliva (spitting on your dick beforehand) and wash your dick and your hands with soap right away afterwards.
Can I get it from rimming?
COVID-19 RNA (the building blocks of the virus) have been found in stool samples (shit) of people who have the virus. But so far, no infectious virus has been found and there are no reported cases of rimming being the cause of passing it on.
Either way, if you’re close enough to rim someone (or get rimmed), you’re close enough to contract it or pass it on through droplets from your/their nose, mouth, or eyes.
Do I have to use condoms?
If you’re close enough to have sex, you’re close enough to get or pass on COVID-19 through droplets, so condoms won’t make a difference there.
BUT now is not a great time to get an STI (as if there’s ever a good time…). There are changes in the delivery of HIV and STI testing and treatment right now. Public health officials are focused on responding to the COVID-19 pandemic—including doctors and nurses who may have been providing sexual health care. Use your typical sexual health strategies like PrEP, condoms, and maintaining an undetectable viral load (U=U). And of course, condoms are still effective at limiting the spread of other STIs (yes, even if you’re on PrEP!).
If you do have symptoms of an STI or have had sex with someone who has tested positive for an STI, reach out to your usual health service provider or to your local public health authority. The Ontario Sexual Health Information Line is currently closed because of COVID-19.
Getting Vaccinated
It’s a good idea to get vaccinated against COVID-19 and to get a booster, if you can. The vaccine reduces the likelihood that you will experience severe symptoms if you do end up contracting COVID-19, and it can help reduce the likelihood that you’ll pass it along to others. For more info on booking a vaccine appointment in Ontario, check out the provincial vaccine portal.
While you’re thinking about vaccines, now is a good time to make sure you’re up-to-date on your other immunizations, including Hep A and Hep B and HPV. In particular, HPV is linked to an increase in throat and rectal cancers among gay men.
Alternatives to hooking up:
There are lots of ways to get off while you’re self-isolating:
- Explore self-pleasure—masturbate, use toys, watch (or listen to or read!) porn.
- Sexting, phone sex, and video sex or camming.
- Have sex with someone you live with (if you’re both interested, of course).
I live alone and can’t handle isolation. What can I do?
Loneliness is very real, and when social spaces are shut down, isolation can have pretty severe effects.
While the main ask from all three levels of government is to stay home, that doesn’t mean that you can’t interact with people. Beyond online and phone connection, it is fine to talk to your neighbours and friends at a distance (2m or more) outside and not in large groups (more than five people).
The key with all of these physical distancing guidelines is to reduce the likelihood that COVID-19 transmission will happen, so work within that.
Drug use / PnP in a pandemic
This is a really important time for drug users to be extra careful. If you’re using alone, the risk of an overdose is very high. If you’re using with others, you may get or pass on COVID-19. If you’re about to use drugs, you can call the Overdose Prevention Line at 1-888 -853-8542 and an operator will stay with you on the phone line while you use drugs.
You may also decide to take this time to cut back or stop all together. If that is something you’re considering, reach out to a medical professional to get advice on the best way to cut back on use safely. If you are going to use drugs during the pandemic, please follow these guides to reduce harm and the risk of transmission:
Wash your hands:
With soap and hot water vigorously for at least 20 seconds (but longer if you can) every time you come into contact with others, after taking public transit or a taxi, after handling money and after you get your drugs. Use paper towels to dry your hands, or at least use a clean towel. If you don’t have access to soap and hot water, an alcohol-based hand sanitizer is the next best thing.
Don’t share:
Sharing drug equipment increases the risk of COVID-19 transmission. This means pipes, bongs, vapes or joints, nasal tubes, and all injecting equipment including: sterilized water, cookers, filters, wipes, ties, etc.
On Opioid Agonist Therapy/Methadone/Suboxone?
If you are on OAT or prescribed opioids for safer supply reasons, ask your doctor if you can get an extended prescription for 1 month. Ask if you can skip appointments and urine testing for at least one month.
Stock-up on drug-using equipment/materials:
Get enough supply to last you at least 3-4 weeks (longer if you are high risk for COVID-19 infection and if programs can manage it), as long as it is safe for you to do this and to have this amount available to you. Stock up on Naloxone as well.
Prepare your drugs yourself:
Always prepare your own drugs yourself, don’t touch or handle other people’s equipment/drugs, and don’t let them touch yours.
Avoid putting drug bags/wraps in your mouth, front hole/vagina, or anus (asshole):
If you have to carry it in your body, clean the drug packaging vigorously with an alcohol-based cleanser both before you put it in and after you take it out. If you carried it in your mouth, use an alcohol-based mouthwash afterwards.
Be ready to go through involuntary withdrawal:
If your supplier(s) get sick or can’t meet you for whatever reason, have back-up plans and make sure you have all the necessary medications, food, and drinks you’ll need to detox off opiates. Similar steps can be taken by those who use other drugs.
HIV and COVID-19
From what we know so far, people living with HIV who are on treatment and are undetectable or otherwise healthy are at no greater risk of contracting COVID-19.
People with HIV who have not been diagnosed or are not on treatment, or those who have a low CD4 count are at a much greater risk of complications related to COVID-19.
For more information on COVID-19 and HIV or Hepatitis C, visit CATIE.ca.

Starting, stopping, and refilling PrEP
PrEP is not an effective treatment or prevention tool for COVID-19. It is still, however, a very effective prevention tool for HIV prevention.
If you’re currently on PrEP and need a refill, talk to your doctor or health service provider as soon as possible. When refilling your prescription, remember that many pharmacies in Ontario are only dispensing one month’s worth of drugs as a way of managing supply.
Some of us who are on PrEP and aren’t having sex are using this time to take a break from it. If you’re considering taking a break, make sure you stop and start your usage correctly.
If you’re a cis guy, keep taking PrEP for another two days after you last had sex. If you’re a trans guy, keep taking PrEP for another seven days after you last had sex.
To re-start your PrEP use, if you haven’t had sex since your last PrEP dose then you can start taking it as usual.
For cis men, if you’re going to have sex right but haven’t been taking your daily dose, you can take a double dose (two pills) of PrEP two to 24 hours before sex. After that, continue with a daily dose—it’s very important to continue to take your usual dose after sex as well.
For trans guys, you’ll need to take a daily dose of PrEP for seven days before you have sex so that you have appropriate front hole/vaginal protection. After that, continue with a daily dose—it’s very important to continue to take your usual dose after sex as well.
If you had sex after you stopped taking PrEP and might have been exposed to HIV, you should get an HIV test before re-starting PrEP. Contact your usual testing facility or your local public health authority to find out where to get an HIV test.
Find more information on the Ontario PrEP site.
Info for sex workers
Hundreds of thousands of Canadians are now out of work as a result of COVID-19-related closures. Sex workers are no exception to that, with the nature of the work putting them at very high risk of contracting or passing on the virus.
Many people are facing cancellations and very real income trouble. Some sex workers have gone online or found other ways to reach their clients, starting their own subscription-based video services.
Organizations like Maggie’s in Toronto are coordinating support for sex workers, including a community fund and a resource guide.
When “home” isn’t safe
The global call to “stay home” is one of the most effective ways to curb the spread of COVID-19. But for GBTQ2S guys, where we live isn’t always safe. Often that’s because we live with hostile family members or roommates or are in insecure or transitional housing. Staying isolated has a bigger impact on you when your living space isn’t safe or stable. Reach out to others if you need support.
Showing up for each other
This is a weird time, to say the least. For many of us, this is the first time we’ve faced this big of a disruption in our daily lives. It can be a lot to handle, and our usual coping strategies might not be available. People are experiencing grief, anxiety, depression, and loneliness. But we’re also seeing a huge outpouring of love and support—in particular online.
Like anything in our society, this has a big impact on the most vulnerable in our communities:
- people who do shift, contract, or sex work
- anyone who works in an “essential” service and doesn’t have paid sick leave
- folks in poverty who can’t afford to stockpile food for weeks
- anyone who relies on public spaces like libraries or community centres
- people who use drugs and risk losing their safety nets
- folks in abusive relationships or unstable housing
- anyone dealing with depression or loneliness

Take care of yourself. Take care of others.
Please do what you need to do to care for yourself during this time. Reach out to others if you’re struggling. If you’re in crisis and are not sure where to go, reach out to the Crisis Text Line.
Here are some other tips for making it through:
- Share a meal over video call with friends or family.
- Check in with others (more than just a “like” on social media).
- Be generous with kind words and love to others who might be alone.
- If you have enough food/resources, make sure others around you do too.
- Offer to order/drop off food or provisions for friends or neighbours.
What is COVID-19?
COVID-19 is a viral respiratory infection caused by a new coronavirus called Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Symptoms can take up to 14 days to start, and can last for several weeks.
- Fever
- Fatigue
- Dry cough
- Difficulty breathing
- Pneumonia in both lungs
For most people, symptoms are mild-to-moderate, if they have symptoms at all.
Some people have more serious complications, and about 15% of people need hospitalization. More serious cases can lead to death.
How is COVID-19 spread?
COVID-19 is most infectious in the first stages, before you produce antibodies & before you may have symptoms. It is spread through droplets (eg. sneezing, coughing, kissing) and is very easily passed on to others.
The biggest factor in transmission is closeness to others. This is why infectious disease experts and doctors are telling people to physically distance themselves from others and to stay at home as much as possible.

It is also possible for the virus to be active on surfaces outside the body for some time—if someone coughs or sneezes, it could be suspended in droplets in the air, or if it’s on someone’s hand and they touch a surface like a door knob or light switch. This is why everyone should be washing their hands with soap frequently and coughing/sneezing either into a tissue or into your elbow.
Who is most at risk?
As a respiratory illness, COVID-19 can cause more complications or serious symptoms in certain people:
- Older people (especially those over 65)
- Smokers (now is a good time to stop, if you’ve been considering it)
- People with other illnesses or conditions
- People living with HIV who have a low CD4 count
- People with limited access to public health services
What if I get sick?
If you think that you may have COVID-19, the first step you should take is to do the Government of Ontario’s self-assessment. The only way to know for sure if you have COVID-19 is with a test. Once you have done the self-assessment, you should call your primary health care provider or, if they are not available (or you don’t have a regular provider), call Telehealth Ontario at 1-866-797-0000 (TTY: at 1-866-797-0007). If Telehealth Ontario isn’t available, you can also reach out to your local public health authority.

Where can I find more information and research about COVID-19?
New information and research are coming out daily on this new virus. To find the most up-to-date information for where you live, visit:
To find the most recent scientific research, visit:
For information about COVID-19 and HIV or Hepatitis C, visit CATIE.ca.
Why physical distancing?
Physical or social distancing is the most effective way to slow the spread of the virus. Because of how quickly it is spread, how severe the symptoms can be, and how quickly complications can develop, hospitals and other healthcare facilities can easily become overwhelmed. That means not having enough space or resources both for people with COVID-19 and for anyone else who needs care.
In places that have experienced this spike, including Iran, Italy, and New York City, the consequences have been major, with unnecessarily high death rates.
Ultimately, the measures we’re taking now are like a global act of love—doing everything we can to reduce the number of people who die from COVID-19 and helping frontline workers manage the situation.
Resources:
- Public Health Agency of Canada
- Ontario Ministry of Health
- Ontario COVID-19 online assessment
- Find your local Public Health Authority
—————
- Telehealth Ontario: 1-866-797-0000 // TTY: 1-866-797-0007
—————
- CATIE: Canada’s source for HIV and Hepatitis C information
- Ontario PrEP
- HIV411
- Health Initiative for Men (HiM Vancouver)
- MPACT: Sex and COVID-19
- PrEPster (UK-based)
—————
- Connex Ontario: Mental health support
- Crisis Text Line: Text HOME to 686868 in Canada to text with a trained Crisis Responder.
- Overdose Prevention Line: 1-888-853-8542
